What Does it Mean if I Have Dense Breasts?
 My Mammogram Letter Says I Have Dense Breasts. What Does That Mean?
My Mammogram Letter Says I Have Dense Breasts. What Does That Mean?
The Ohio legislation passed a new law concerning breast density as it relates to mammography results. This new law requires TriHealth to include the following statement on reports for our patients who have heterogeneously or very dense breasts:
Your mammogram demonstrates that you have dense breast tissue, which could hide abnormalities. Dense breast tissue, in and of itself, is a relatively common condition. Therefore, this information is not provided to cause undue concern; rather, it is to raise your awareness and promote discussion with your health care provider regarding the presence of dense breast tissue in addition to other risk factors.
What is Breast Density and Why is it Important
Breasts are made up of a mixture of fibrous and glandular tissue and fatty tissue. Your breasts are considered dense if you have a lot of fibrous or glandular tissue but not much fat. Density may decrease with age, but there is little, if any, change in most women.
Having dense breast tissue may increase your risk of getting breast cancer. Dense breasts also make it more difficult for doctors to spot cancer on mammograms. Dense tissue appears white on a mammogram. Lumps, both benign and cancerous, also appear white. So, mammograms can be less accurate in women with dense breasts.
How do I Know if I Have Dense Breasts?
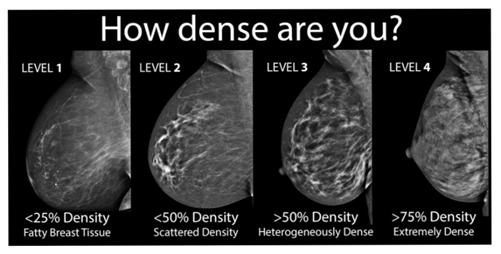
Breast density is determined by the radiologist who reads your mammogram. There are four categories of mammographic density. The radiologist assigns each mammogram to one of the categories.
Imaging Dense Breasts
- Mammography is still the preferred screening method for breast cancer. Women 40 and over should receive annual screening mammograms.
- 3D mammography is a newer technology that is superior for women with heterogeneously dense breasts. This technology is now covered by Medicare, but coverage varies between commercial payers.
- Whole breast ultrasound and breast MRI are both supplementary screening tools for women with extremely dense breast tissue. However, these tests are more sensitive and can identify things that are not cancer, leading to biopsies and other testing that may not be necessary. These tests are also very expensive and often not covered by insurance if not properly justified. For this reason, additional risk evaluation can be a vital part of a thorough risk assessment.
What Does This Mean for You?
If your follow up letter from your recent mammogram notes that you have dense breast tissue, you will fall into one of two categories:
- Heterogeneously dense breast tissue, or
- Extremely dense breast tissue
If you have no other risk factors, your best option may be to have a 3D mammography at your next screening mammogram. TriHealth offers this advanced technology at Bethesda North Hospital at the Mary Jo Cropper Family Center for Breast Care and Good Samaritan Hospital.
Risk Evaluation
Whether your breasts are dense or fatty, there may be other factors that can still place you at increased risk for breast cancer. These include:
- Family history of the disease
- Previous chest radiation treatment for cancer
- Previous breast biopsies that show you are high risk
It is important to understand your risk factors and discuss them with your physician. There are several models to assess your risk.
You can determine your risk factors by consulting with your physician, completing a risk assessment or speaking with one of our counselors at the Breast Center.
- All TriHealth patients are welcome to a free risk assessment through our center by calling 513 862 5160.
Online Breast Cancer Risk Assessment Tool
To further assess your risk for breast cancer, please go to the following website and answer eight simple questions:
This Breast Cancer Risk Assessment Tool is based on a statistical model known as the "Gail model". The model uses the following factors to estimate a woman's risk of developing invasive breast cancer over specific periods of time:
- Her own personal medical history
- Her own reproductive history
- History of breast cancer among her first-degree relatives (mother, sisters, and daughters)
The Gail model has been validated in large populations of white women and performs well in other populations such as African American women with previous biopsies, Asian and Pacific Islanders, but needs further validation for Hispanic women and other subgroups.
The Gail model may underestimate the risk of breast cancer if there is a history of breast cancer on your father's side, relatives who are beyond first degree (e.g., aunt, grandparent, cousin) or if you have a personal history of breast cancer. If your history contains these factors, you should speak with your physician about the appropriate risk assessment and screening plan for you. Patients with extensive family history of cancer (e.g., breast, ovarian, pancreatic, colon, with 3 affected family members or with a diagnosis under the age of 50) can find additional information about genetic counseling here, (add hyperlink) or may request a genetic counseling consultation by calling 513 451 4033, option 1.
After completing the questionnaire, you will be able to print your breast cancer risk assessment and take to your physician for further discussion. Your doctor can help you determine if further screening or testing is necessary. The TriHealth Breast Care team is also available to answer questions and can be reached at 513 862 5160.
Genetic Counseling
The goal of genetic counseling is to provide personalized information about an individual’s cancer risk factors, genetic testing options, and recommendations for cancer screening, treatment and management. The genetic counselor will take a complete family history and medical history. During the risk assessment the patient will learn more about their cancer risk and potential risk to other family members.
For further questions about breast density, risk assessments, or supplementary imaging, please call 513 862 5160 and we will be happy to assist you!